How to Prevent Gallstones from Forming? | Natural Supplements for Gallstones
How To Prevent Gallstone Formation?
Gallstones are hard deposits made of cholesterol or bilirubin found in bile. Gallstones can develop in the gallbladder or bile ducts. Bile is produced by the liver and flows into the gallbladder to be stored and released to help with the digestion and absorption of fat . Gallstones are commonly formed due to excessive amounts of cholesterol in the bile which causes bile to thicken and crystallize.
Gallstones are formed in a variety of sizes, from tiny grains of sand to golf ball-sized particles. Often those small stones cause the most trouble. These little stones can leave the gallbladder and get trapped in the bile duct. Larger stones tend to remain in the gallbladder. Many people who have gallstones are never bothered by them and may not be aware of their formation.
Gallstones cause inflammation of the gallbladder which manifests itself in the form of dull pain and indigestion. Moving stones, however, result in acute and often severe pain if they block bile flow. Gallstones may result in inflammation of the gallbladder, liver, or pancreas and in rare occasions may become life-threatening.Gallstones are also linked to increased risk of certain cancers and cardiovascular diseases.
What is the gallbladder?
The gallbladder is a small pear shaped, muscular pouch beneath the liver, on the right side of the body. It is about three to six inches long. The gallbladder’s job is to receive, store, and dispense bile produced by the liver cells.
Bile moves through a network of small ducts within the liver. The connection of these small ducts forms the right hepatic duct (which drains bile from the right half of the liver) and the left hepatic duct (which drains bile from the left half of the liver). The junction of the left and right hepatic ducts forms the common hepatic duct. The common hepatic duct from one side is connected directly to the common bile duct and the duodenum (the first part of the small intestine); while from another side, it connects to cystic duct leading to the gallbladder. This entire system of ducts is called the biliary system.
The gallbladder stores bile, which is available to be used for digestion on very short notice. Between meals, the gallbladder is relaxed, but during meals, signals from the digestive tract stimulate contractions of the gallbladder and some stored bile is released into the common bile duct where it’s passed into the small intestine to mix with food.
What is bile?
Bile is a dark-green-to-yellowish-brown fluid which is continuously produced by the liver. It is a combination of cholesterol, bilirubin, bile salts and lecithin. Bile helps break down fat during the digestion process. Bile reaches the duodenum directly from the hepatic duct (from the liver) or from the gallbladder.
Bile in addition to being an important part of digestion, carries waste products from the liver to be eliminated through the digestive tract
The two main pigments of bile are bilirubin, which is orange–yellow, and its oxidized form biliverdin which is green. When mixed, they are responsible for the brown colour of the stool.
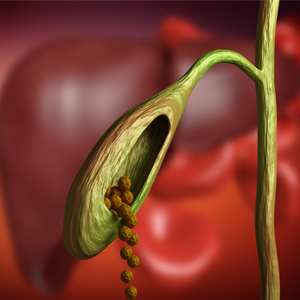
What are the gallstones?
Gallstones are hard deposits formed from bile components. Gallstones can be categorized based on their cholesterol content:
Cholesterol stones; are usually made up of more than 70 % cholesterol and are the most common type of gallstones.
Pigment Stones; are mainly made of bilirubin and formed due to high levels of bilirubin. Pigment stones contain less than 30 % cholesterol. Calcium salts are also found in higher concentrations in pigment gallstones.
Pigment stones usually form when there is increased level of bilirubin in the bile. Conditions such as liver cirrhosis, certain blood disorders, parasitic infections, and narrowing of bile ducts can cause increased bilirubin in the bile, contributing to pigment gallstones formation.
Mixed stones; are referred to the stones with the cholesterol content between 30% and 70%.
Majority of gallstones are cholesterol stones or mixed stones which are linked to diets consisting of high amounts of cholesterol and saturated fats. People with gallstones often have high levels of oxidized lipids in their blood.
At the very beginning stage of the stone formation, gallbladder muscles are weakened which reduces the gallbladder response to the signals from digestive tract to empty the bile. Therefore, the thicken bile and the cholesterol sludge remain in the gallbladder to create gallstones over time.
Gallstones are most found in the gallbladder, but they can travel from the gallbladder to the common bile duct, which is the largest duct in the liver.
What conditions are associated with gallstones?
The bile duct stones are much less common but can create more serious medical situations than just gallstones that stay in the gallbladder. Common bile duct stones can block the common bile duct, resulting in a serious infection known as cholangitis; inflammation of the gallbladder, pancreatitis (inflammation of the pancreas), and Choledocholithiasis occur when one or more gallstones trapped in the common bile duct. Biliary pain is the most common symptom of gallstone disease, which is commonly described as acute, severe pain in the upper-right or upper-mid region of the abdomen, radiating to the right shoulder or between the shoulder blades; and it may last for minutes to hours especially after eating.
Cholecystitis (inflammation of the gallbladder) causes biliary pain, fever, and nausea. In its chronic form causes digestive symptoms such as gas, bloating, nausea, and gag. These symptoms are usually worse after eating fatty foods.
cholangitis is Infection& inflammation of the bile ducts due to an obstruction, causing abdominal pain, fever, and jaundice.
pancreatitis is the inflammation of the pancreas due to blockage of the pancreatic duct. It symptoms include biliary pain , and potential life-threatening condition in which causes the inflammation of the lining of the inner abdominal wall (peritonitis).
Ileus is another rare condition that can be caused by larger stones. Ileus is the lack of intestinal movement that leads to a buildup with potential blockage of food material, and an intestinal obstruction. This means no food material, gas, or liquids can not get through.
Why do the gallstones form?
Gallstones can develop for several reasons involving genetic, ethnicity, gender, age, family history, diet, and environmental factors. When there is a critical concentration of cholesterol or bilirubin in the bile, slow gallbladder that does not empty the bile, liver diseases, blood disorders, aging, during pregnancy, rapid weight loss, fasting, obesity, high blood sugar or diabetes, high blood lipids, hormonal imbalance, hormone therapy, and certain medications increase the risk of gallstone formation.
High caloric foods, carbohydrates, saturated fats, and sugar along with low intake of fiber have been linked to increased risk, while consumption of polyunsaturated fats, fiber, fish, fruits and vegetables, and nuts have been associated with lower risk.
While gradual weight loss may reduce gallstone risk, rapid weight loss increases the risk of gallstone formation. Prolonged fasting and weight cycling often seen in inconsistent dieting are also contribute to higher cholesterol gallstone risk.
Evidently, food allergies and intolerances promote gallstone formation by triggering gallbladder inflammation and slowing gallbladder emptying. One week of the elimination diet helped to resolve the gallbladder symptoms in all participants. Suspected food allergens such as dairy (milk, cheese, and ice cream), wheat (gluten), soy, corn, preservatives, and chemical food additives, and Eggs, especially, may irritate the gallbladder. Your practitioner may recommend testing for food allergies.
Risk of developing cholesterol and pigmented stones increases with age, due to lower bile acid production which is leading to greater concentration of cholesterol in the gallbladder. Also, aging may also be associated with reduced gallbladder motility.
Additional hormone exposure through oral contraceptives and post-menopausal hormone therapy may increase the risk of gallstone formation. Data analysis suggests that that hormone therapy increased risk of gallstones. Estrogen seems to be responsible for this negative effect, and adding the progesterone to estrogen therapy does not reduce the risk. Topical bioidentical estradiol also demonstrated the same negative effect on bile cholesterol saturation and crystallization time after eight weeks of use.
Gallstones are more common during pregnancy due to decreased gallbladder motility and increased cholesterol saturation of bile. Added estrogen in the body can lead to an increased amount of cholesterol in the bile, while also reducing gallbladder contractions (cholestasis of pregnancy).
Individuals with iron-deficiency anemia are at a higher risk of gallstones than those with normal iron levels. This relationship has been verified in the reverse as well: gallstone patients have been found to be more likely to have low serum iron levels than healthy individuals . Iron deficiency may alter the activities of several liver enzymes, leading to increased cholesterol saturation in bile and increased cholesterol crystallization, and it also negatively impacts gallbladder motility. In addition, it is possible that gallstone disease contributes to iron malabsorption and poor iron status. Only those with iron deficiency should consider iron supplementation to reduce the risk of gallstones.
High levels of iron due to break don of red blood cells in certain diseases and also due to high intake of specially Heme iron or Iron from the red meat is associated with higher risk of pigment gallstone formation.
Several pharmaceuticals are known to increase the risk of gallstones, such as estrogens, oral contraceptives, anti-biotics, diuretics (used mainly to treat high blood pressure), and some blood cholesterol lowering agents.
Which natural medicine can help prevent gallstone formation?
Individuals with higher risk factors of ethnicity, age, family history, hormone therapy, or medical factors such as high blood lipids (cholesterol & triglycerides), high blood sugar, liver conditions like none alcoholic fatty liver, viral hepatitis, or history of some parasitical infections, slow digestion, dyspepsia, gas, bloating, and those with known silent gallstones, or the history of them may want to consider supplements to reduce their risk.
Vitamin C is necessary for the conversion of cholesterol into bile acids . The link between vitamin C deficiency and gallstones has been recognized decades ago. Low vitamin C level causes increased cholesterol saturation in the bile. In a group of candidate of gallbladder removal those who supplemented with vitamin C showed better bile consistency and delayed formation of further cholesterol crystals than those without vitamin C.
Supplementing with omega-3 fatty acids of high EPA and DHA may help prevent gallstones by improving bile composition and the gallbladder function.
A study looked at gallbladder function in individuals with obesity and high insulin levels found that those who took omega3 supplement or ate fish had a better gallbladder function than those who did not, concluding omega 3 helps lowering their risk for gallbladder problems.
Omega-3 helps to encourage the gallbladder to empty itself regularly, something that is considerably helpful if an individual also has high triglyceride levels which have been associated with gallstone development. Supplementing for roughly six weeks makes a difference in how the gallbladder is reacting.
Data from other studies suggest that supplementing with 3.7g omega 3 daily helped to reduce the ratio of cholesterol to phospholipids in bile; and lowered super saturation with cholesterol, thus helped to prevent precipitation of cholesterol crystals in bile of gallstone patients.
S-Adenosyl-L-Methionine (SAMe) is a natural compound and methyl group donor that supports the methylation cycle, glutathione production, and gene expression. Methylation is fundamental for the elimination of certain toxins. Chronic liver disorders and alcohol consumption inhibit the ability to produce an adequate amount of SAMe. SAMe supplementation helps to improve the bile flow. SAMe is also beneficial for women with an increased bile cholesterol saturation after starting oral contraceptives; supplementing with SAMe for two cycles has helped to reduce the bile cholesterol saturation in participants.

Curcumin helps reduce the possibility of gallstone formation by improving cholesterol and lipid metabolism. Curcumin has also been shown to improve gallbladder motility, reduce gallbladder inflammation, and normalize bile acid metabolism. Curcumin may also be helpful in recovery after cholecystectomy and reduces the need for pain relievers.
Milk thistle is often used as a natural treatment for liver conditions such as cirrhosis, jaundice, hepatitis, and gallbladder disorders. Silymarin is the main active ingredient in milk thistle. Silymarin provides both anti-inflammatory and antioxidant benefits. Silymarin and silybin, its major active compound, have been noted to reduce bile cholesterol content in human, suggesting its potential value in gallstone prevention and treatment. Milk thistle in general is considered safe and well-tolerated .
Dandelion is regarded one of the finest liver remedies. It enhances the flow of bile, and helps improving liver congestion, bile duct inflammation, hepatitis, gallstones, and jaundice. Supplementing with dandelion root extract helps to increase bile production in the liver causing greater flow of bile to the gallbladder (choleretic effect). In addition, it causes contraction and release of stored bile in the gallbladder (cholagogue effect).
The active ingredient in Artichoke is cynarin, which like silymarin demonstrates significant liver protective and regenerative effects. It also creates a choleretic effect, with acts to decongest the liver.
The other most common natural medicine for the liver diseases is the artichoke (Cynara scolymus L., family Asteraceae. Cynarin is one of the important bioactive constituents of artichoke. Clinical treatments have confirmed the therapeutic properties of this plant, especially in hypercholesterolemia, digestive disorders and irritable bowel syndrome. Currently, the raw material is used for the production of medicinal preparations for liver failure, inflammation of the gallbladder, cholangitis, cholelithiasis and disorders of lipid metabolism. Furthermore, it was shown that extracts from artichoke leaves indirectly reduces hepatic cholesterol biosynthesis.
Cynarin compound stimulates bile secretion and helps to reduce blood cholesterol which in turn helps prevent gallstones forming, it said in a press release.
A high-fiber diet helps prevent gallstones. In several publications, it has been recommended for women to take 25 grams of fiber daily and men consume 38 grams of fiber.
Those who followed the high fiber diet accumulated less gallbladder sludge, which reduced their risk of developing gallbladder disease. This suggests that a high fiber diet can help prevent gallbladder disease in individuals who need to lose weight quickly, and perhaps overall.
Results from clinical studies have supported effectiveness of specific homeopathic remedies. However, a professional homeopath may recommend one or more of the treatments for gallbladder disease based on clinical experience considering totality of person's signs and symptoms including all the physical plus emotional status of the patient to choose appropriate treatment plan.
Some of the most common homeopathic medicines for gallbladder conditions are including; Colocynthis, for colicky abdominal pains which get better by pressure or bending. Chelidonium, for when the abdominal pain that radiated to the shoulder area. Lycopodium, for when abdominal pain gets worse with deep breaths. Remedies, doses, and potencies may vary depending on the stage of the condition.

What lifestyle and dietary factors would help to prevent gallstone formation?
Dietary factors are very important when it comes to preventing cholesterol gallstone formation. High calorie diets including high fat, sugar, refined carbohydrates, saturated fat, cholesterol, trans fats, fried foods, highly processed foods (doughnuts, cookies, white bread), High fat dairy products (milk, butter, cheese, ice cream), Processed meats (bacon, ham, sausage), and alcohol increase risk of gallstones and the related complications.
Diet rich in fiber, vegetables, plant based proteins, omega3 fats, , and legumes is associated with lower risks of gallstone formation.
In overweight individuals weight management strategies are very important to reduce the risk of gallstones; however, a rapid weight loss increases the possibility of gallstone formation.
Physical activity may help prevent cholesterol gallstone formation by improving the motility of the digestive system and by helping with cholesterol metabolism.
During pregnancy keeping a healthy diet rich in fiber, Good fats like omega3's and unsaturated fats, and low in refined carbohydrates, and saturated fat such as those found in animal products may help reduce risk of gallbladder symptoms. This can help keep you and your baby healthy. But always keep your healthcare practitioner informed if you do have symptoms that involve your gallbladder.
Related Articles:
- How to Maintain and Restore Healthy Blood Lipids Level
- How to lose weight successfully and maintain it!
- The best way to know your liver and protect it!
- How to maintainhealthy blood sugar & improve diabetic conditions?
Articles and products featured by Health Palace are collected from a variety of sources and are provided as a service by Health Palace. These newsletters, while of potential interest to readers, do not necessarily represent the opinions nor constitute the advice of Health Palace. Presented materials are only for information purposes and do not intent to treat, cure, or prevent any disease.
References:
- Fogel ELS, S. Diseases od the Gallbladder and Bile Ducts. In: Goldman L, Schafer A, eds. Goldman-Cecil Medicine. 25th edition. Philadelphia: Pennsylvania: Elsevier/Saunders; 2016:1038–1048. 2016.
- Housset C, Chretien Y, Debray D, Chignard N. Functions of the Gallbladder. Comprehensive Physiology. Jun 13 2016;6(3):1549-1577.
- Jones MW, Ghassemzadeh S. Gallbladder, Gallstones (Calculi). StatPearls. Treasure Island (FL): StatPearls Publishing LLC.; 2018.
- Hundt M, John S. Physiology, Bile Secretion. StatPearls. Treasure Island (FL): StatPearls Publishing LLC.; 2018.
- University of Maryland Medical Center; Gallstones and Gallbladder Disease - Risk Factors; June 26, 2009
- Jiang ZY, Sheng X, Xu CY, et al. Gallbladder gallstone disease is associated with newly diagnosed coronary artery atherosclerotic disease: a cross-sectional study. PLoS One. 2013;8(9):e75400.
- International Journal of Clinical Chemistry"; Triglycerides and Gallstone Formation; A. Smelt; November 2010
- https://europepmc.org/article/med/1398503 gallstone disease.
- Kaufman HS, Magnuson TH, Pitt HA, Frasca P, Lillemoe KD. The distribution of calcium salt precipitates in the core, periphery and shell of cholesterol, black pigment and brown pigment gallstones. Hepatology. May 1994;19(5):1124-1132.
- Vitek L, Carey MC. New pathophysiological concepts underlying pathogenesis of pigment gallstones. Clinics and research in hepatology and gastroenterology. Apr 2012;36(2):122-129.
- Chen Y, Kong J, Wu S. Cholesterol gallstone disease: focusing on the role of gallbladder. Laboratory investigation; a journal of technical methods and pathology. Feb 2015;95(2):124-131.
- Di Ciaula A, Wang DQ, Bonfrate L, Portincasa P. Current views on genetics and epigenetics of cholesterol gallstone disease. Cholesterol. 2013;2013:298421.
- Wang HH, Liu M, Li X, Portincasa P, Wang DQ. Impaired intestinal cholecystokinin secretion, a fascinating but overlooked link between coeliac disease and cholesterol gallstone disease. European journal of clinical investigation. Apr 2017;47(4):328-333.
- Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut and liver. Apr 2012;6(2):172-187.
- Ko, CW. Prefac: Gallbladder disease. Gastroenterol Clin North Am. 2010;39(2):xiii.
- Shaffer EA. Gallstone disease: Epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol. 2006;20(6):981-96.
- Karłowicz-Bodalska K, Bodalski T. Role of plant crude drugs in treatment of liver diseases. Post Fitoter 2007; 3:155-167.
- Boroń-Kaczmarska A, Morańska I, Kruszewski T. Hepatic disorders, therapy recommendations. Nowa Klin 1999; 6(1):45-48.
- Krauze M. Arnika, karczoch, kozieradka w laboratorium. Panacea 2004; 2(7):32.
- Gawęcki J, Hryniewiecki L. Żywienie człowieka. Podstawy nauki o żywieniu. Wydawnictwo PWN S.A., Warszawa 2004; 198-206.
- Baiu I, Hawn M. Gallstones and Biliary Colic. JAMA. 2018; 320(15): 1612. Accessed 10/15/2019.
- US Department of Health and Human Services, National Institute of Diabetes and Digestive and Kidney Diseases. Gallstones. Accessed 10/15/2019.
- US Department of Health and Human Services, National Institute of Diabetes and Digestive and Kidney Diseases. Endoscopic Retrograde Cholangiopancreatography (ERCP). Accessed 10/15/2019.
- American Academy of Family Physicians. Gallstones. Accessed 10/15/2019.
- Nemours, KidsHealth. A to Z: Cholelithiasis (Gallstones). Accessed 10/15/2019.
- American Family Physician. Gallstones: What are they? How are they treated? Accessed 10/15/2019.
- American Gastroenterological Association. Gallstones. Accessed 10/15/2019.
- Merck Manual. Gallstones. Accessed 10/15/2019.
- American Heart Association. Cooking to Lower Cholesterol. Accessed 10/15/2019.
- Could Your Abdominal Pain Actually Be Gallstones? Cleveland Clinic. May 13, 2019.
- Gallstones. National Institute of Diabetes and Digestive and Kidney Diseases.
- Bari O, Wang T, Liu M, Paik C, Portincasa P, Wang D. Cholesterol cholelithiasis in pregnant women: Pathogenesis, prevention and treatment. Ann Hepatol. 2014;13(6):728-745. doi:10.1016/s1665-2681(19)30975-5
- Jessri, M. & Rashidkhani, B. (2015). Dietary patterns and risk of gallbladder disease: A hospital-based case-control study in adult women. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4438...
- Lander, E. M., et al. (2016). Vegetable protein intake is associated with lower gallbladder disease risk: Findings from the Women’s Health Initiative prospective cohort. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4902...
- Stokes CS, Gluud LL, Casper M, Lammert F. Ursodeoxycholic acid and diets higher in fat prevent gallbladder stones during weight loss: a meta-analysis of randomized controlled trials. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. Jul 2014;12(7):1090-1100.e1092; quiz e1061.
- Erlinger S. Gallstones in obesity and weight loss. European journal of gastroenterology & hepatology. Dec 2000;12(12):1347-1352.
- Fraquelli M, Pagliarulo M, Colucci A, Paggi S, Conte D. Gallbladder motility in obesity, diabetes mellitus and coeliac disease. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver. Jul 2003;35 Suppl 3:S12-16.
- Overview: Gallstones. (2018). https://www.nhs.uk/conditions/gallstones/.
- Sulaberidze, G., et al. (2014). Dietary fiber’s benefit for gallstone disease prevention during rapid weight loss in obese patients [Abstract]. https://www.ncbi.nlm.nih.gov/pubmed/25020181
- Fraquelli M, Pagliarulo M, Colucci A, Paggi S, Conte D. Gallbladder motility in obesity, diabetes mellitus and coeliac disease. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver. Jul 2003;35 Suppl 3:S12-16.
- Lee HS, Chung MJ, Park JY, Bang S, Park SW, Song SY, Chung JB. Urgent endoscopic retrograde cholangiopancreatography is not superior to early ERCP in acute biliary pancreatitis with biliary obstruction without cholangitis. PloS one. 2018;13(2):e0190835.
- Zimmer V, Lammert F. Acute Bacterial Cholangitis. Viszeralmedizin. Jun 2015;31(3):166-172.
- Setiawan VW, Pandol SJ, Porcel J, Wei PC, Wilkens LR, Le Marchand L, . . . Monroe KR. Dietary Factors Reduce Risk of Acute Pancreatitis in a Large Multiethnic Cohort. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. Feb 2017;15(2):257-265.e253.
- Turner AR, Bhimji SS. Ileus, Gallstone. StatPearls. Treasure Island (FL): StatPearls Publishing LLC.; 2018.
- Di Ciaula A, Wang DQ, Bonfrate L, Portincasa P. Current views on genetics and epigenetics of cholesterol gallstone disease. Cholesterol. 2013;2013:298421.
- Macias B, Gomez-Pinilla PJ, Camello-Almaraz C, Pascua P, Tresguerres JA, Camello PJ, Pozo MJ. Aging impairs Ca(2+) sensitization pathways in gallbladder smooth muscle. Age. Aug 2012;34(4):881-893.
- Wang S, Wang Y, Xu J, Chen Y. Is the oral contraceptive or hormone replacement therapy a risk factor for cholelithiasis: A systematic review and meta-analysis. Medicine. Apr 2017;96(14).
- Wang F. Oral contraceptives and risk of gallbladder disease. CMAJ. 2011:183(13):1517
- Breneman JC. Allergy elimination diet as the most effective gallbladder diet. Annals of allergy. Feb 1968;26(2):83-87.
- Dhiman RK, Chawla YK. Is there a link between oestrogen therapy and gallbladder disease? Expert opinion on drug safety. Jan 2006;5(1):117-129.
- Simonsen MH, Erichsen R, Froslev T, Rungby J, Sorensen HT. Postmenopausal estrogen therapy and risk of gallstone disease: a population-based case-control study. Drug safety. Dec 2013;36(12):1189-1197.
- Liu B, Beral V, Balkwill A. Childbearing, breastfeeding, other reproductive factors and the subsequent risk of hospitalization for gallbladder disease. Int J Epidemiol. 2009;38(1):312-8.
- Gaby AR. Nutritional approaches to prevention and treatment of gallstones. Altern Med Rev. 2009:14(3):258-67.
- Walcher T, Haenle MM, Kron M, Hay B, Mason RA, Walcher D, . . . Kratzer W. Vitamin C supplement use may protect against gallstones: an observational study on a randomly selected population. BMC gastroenterology. Oct 8 2009;9:74.
- del Pozo R, Munoz M, Dumas A, Tapia C, Munoz K, Fuentes F, . . . Jungst D. [Effects of vitamin C administration on cholesterol gallstone formation]. Revista medica de Chile. Jan 2014;142(1):20-26.
- Ginter E. Cholesterol: vitamin C controls its transformation to bile acids. Science (New York, N.Y.). Feb 16 1973;179(4074):702-704.
- Gustafsson U, Wang FH, Axelson M, Kallner A, Sahlin S, Einarsson K. The effect of vitamin C in high doses on plasma and biliary lipid composition in patients with cholesterol gallstones: prolongation of the nucleation time. European journal of clinical investigation. May 1997;27(5):387-391.
- Simon JA, Hudes ES. Serum ascorbic acid and gallbladder disease prevalence among US adults: the Third National Health and Nutrition Examination Survey (NHANES III). Archives of internal medicine. Apr 10 2000;160(7):931-936.
- Simon JA, Hudes ES. Serum ascorbic acid and other correlates of gallbladder disease among US adults. American journal of public health. Aug 1998;88(8):1208-1212.
- Worthington HV, Hunt LP, McCloy RF, Maclennan I, Braganza JM. A pilot study of antioxidant intake in patients with cholesterol gallstones. Nutrition (Burbank, Los Angeles County, Calif.). Feb 1997;13(2):118-127.
- Walcher T, Haenle MM, Kron M, Hay B, Mason RA, Walcher D, . . . Kratzer W. Vitamin C supplement use may protect against gallstones: an observational study on a randomly selected population. BMC gastroenterology. Oct 8 2009;9:74.
- Jonkers IJ, Smelt AH, Princen HM, Kuipers F, Romijn JA, Boverhof R, . . . Stellaard F. Fish oil increases bile acid synthesis in male patients with hypertriglyceridemia. The Journal of nutrition. Apr 2006;136(4):987-991.
- Mendez-Sanchez N, Gonzalez V, Aguayo P, Sanchez JM, Tanimoto MA, Elizondo J, Uribe M. Fish oil (n-3) polyunsaturated fatty acids beneficially affect biliary cholesterol nucleation time in obese women losing weight. The Journal of nutrition. Sep 2001;131(9):2300-2303.
- Berr F, Holl J, Jungst D, Fischer S, Richter WO, Seifferth B, Paumgartner G. Dietary N-3 polyunsaturated fatty acids decrease biliary cholesterol saturation in gallstone disease. Hepatology. Oct 1992;16(4):960-967. Hepatology (Baltimore, Md.), 30 Sep 1992, 16(4):960-967 DOI: 10.1002/hep.1840160418 PMID: 1398503 .
- Cho SM, Park JA, Kim NH, Kim DS, Zhang D, Yi H, . . . Shin HC. Effect of eicosapentaenoic acid on cholesterol gallstone formation in C57BL/6J mice. Molecular medicine reports. Jan 2015;11(1):362-366.
- Almasio P, Bortolini M, Pagliaro L, Coltorti M. Role of S-adenosyl-L-methionine in the treatment of intrahepatic cholestasis. Drugs. 1990;40 Suppl 3:111-123.
- Worthington HV, Hunt LP, McCloy RF, Ubbink JB, Braganza JM. Dietary antioxidant lack, impaired hepatic glutathione reserve, and cholesterol gallstones. Clinica chimica acta; international journal of clinical chemistry. Nov 2004;349(1-2):157-165.
- Di Padova C, Tritapepe R, Di Padova F, Frezza M, Stramentinoli G. S-adenosyl-L-methionine antagonizes oral contraceptive-induced bile cholesterol supersaturation in healthy women: preliminary report of a controlled randomized trial. The American journal of gastroenterology. Dec 1984;79(12):941-944.
- Frezza M, Tritapepe R, Pozzato G, Di Padova C. Prevention of S-adenosylmethionine of estrogen-induced hepatobiliary toxicity in susceptible women. The American journal of gastroenterology. Oct 1988;83(10):1098-1102.
- Li Y, Li M, Wu S, Tian Y. Combination of curcumin and piperine prevents formation of gallstones in C57BL6 mice fed on lithogenic diet: whether NPC1L1/SREBP2 participates in this process? Lipids in health and disease. Sep 3 2015;14:100.
- Rasyid A, Lelo A. The effect of curcumin and placebo on human gall-bladder function: an ultrasound study. Alimentary pharmacology & therapeutics. Feb 1999;13(2):245-249.
- Rasyid A, Rahman AR, Jaalam K, Lelo A. Effect of different curcumin dosages on human gall bladder. Asia Pacific journal of clinical nutrition. 2002;11(4):314-318.
- Shubha MC, Reddy RR, Srinivasan K. Antilithogenic influence of dietary capsaicin and curcumin during experimental induction of cholesterol gallstone in mice. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. Apr 2011;36(2):201-209.
- Yang F, Tang X, Ding L, Zhou Y, Yang Q, Gong J, . . . Yang L. Curcumin protects ANIT-induced cholestasis through signaling pathway of FXR-regulated bile acid and inflammation. Scientific reports. Sep 14 2016;6:33052.
- Crocenzi FA, Sanchez Pozzi EJ, Pellegrino JM, Favre CO, Rodriguez Garay EA, Mottino AD, . . . Roma MG. Beneficial effects of silymarin on estrogen-induced cholestasis in the rat: a study in vivo and in isolated hepatocyte couplets. Hepatology. Aug 2001;34(2):329-339.
- Natural Medicines Comprehensive Database: "Milk Thistle Monograph." National Center of Complementary and Alternative Medicine (NCCAM): "Milk Thistle."
- Pittler MH, Thompson CO, Ernst E. Artichoke leaf extract for treating hypercholesterolemia. (Cochrane Review). In: The Cochrane Library, Issue 1, Oxford, 2006.
- Sulaberidze G, Okujava M, Liluashvili K, Tughushi M, Bezarashvili S. Dietary fiber's benefit for gallstone disease prevention during rapid weight loss in obese patients. Georgian medical news. Jun 2014(231):95-99.
- Di Ciaula A, Garruti G, Fruhbeck G, De Angelis M, De Bari O, D QHW, . . . Portincasa P. The Role Of Diet In The Pathogenesis Of Cholesterol Gallstones. Current medicinal chemistry. May 29 2017.
- Aune D, Leitzmann M, Vatten LJ. Physical Activity and the Risk of Gallbladder Disease: A Systematic Review and Meta-Analysis of Cohort Studies. Journal of physical activity & health. Jul 2016;13(7):788-795.
- Walcher T, Haenle MM, Mason RA, et al. The effect of alcohol, tobacco and caffeine consumption and vegetarian diet on gallstone prevalence. Eur J Gastroenterol Hepatol. 2010;22(11):1345-51.
Recent Posts
-
Macular degeneration
Macular degeneration which is commonly known as age-related macular degeneration (AMD /ARMD), is a m …7th Sep 2025 -
Maintain A Healthy Heart Rhythm With Integrative Medicine
Maintain A Healthy Heart Rhythm With Integrative Medicine;Usually, abnormal heart rate or arrhythmi …4th Feb 2021 -
How to Prevent Gallstones from Forming? | Natural Supplements for Gallstones
How To Prevent Gallstone Formation?Gallstones are hard deposits made of cholesterol or bilirubin f …4th Mar 2020



