10 Ways to Boost your Heart Health | How to Improve Heart Health Naturally?
What is Homocysteine & How Is It Related to Cardiovascular Disease
Cardiovascular conditions affect one-third of the population worldwide and have remained among the top concerns in medical society. Alongside medical advancements, surgical techniques, and drugs, safe and effective preventive methods provide the most suitable way for the reduction in Cardiovascular Disease (CVD). A healthy lifestyle including physical activity and stress management, nutrition, and the elimination of the risks of atherosclerosis (smoking, diabetes, hypertension, obesity, elevation of plasma cholesterol, and homocysteine) all contribute to the primary prevention of CVD. As an example, elevated Homocysteine is considered a risk factor for Cardiovascular Disease while it can be lowered and kept at safe levels to prevent arterial damage and its unwanted adverse effects.
What Is Homocysteine?

Homocysteine is a sulfur (sulfhydryl) containing amino acid which is naturally produced as a result of our body using dietary amino acid Methionine to produce amino acid Cysteine. Methionine is an essential amino acid for humans and is found in high amounts in animal proteins including meat, egg, and dairy products. In the event of Methionine deficiency, Homocysteine can be recycled to make more Methionine, while in the presence of enough Methionine, it will be turned into Cysteine.
A high blood level of homocysteine (hyperhomocysteinemia) may arise from genetic defects of enzymes involved in homocysteine metabolism and/or from nutritional deficiencies of folate, vitamin B6, and vitamin B12. In addition; several diseases such as kidney and thyroid disorders, cancer, psoriasis, and diabetes as well as some types of drugs, alcohol, tobacco, coffee, older age, and menopause, are found to be associated with moderately high homocysteine levels. High serum creatinine is indicative of kidney disease which also leads to elevated fasting total homocysteine.
Plasma homocysteine is mainly cleared via kidneys, therefore any kidney disorder may impact the homocysteine blood concentrations. Total homocysteine levels are found to be considerably higher in patients with chronic renal disease. Plasma homocysteine can be increased by drugs and diseases that interfere with metabolism and or absorption of B vitamins especially folate, vitamin B6, and B12.
Correlation Between High Blood Homocysteine Level & Cardiovascular Disease
Homocysteine is known as an independent risk factor for Atherosclerosis (hardening of the arteries). Also; higher blood homocysteine level enhances the adverse effects of cardiovascular disease risk factors such as high blood pressure, high blood lipids, smoking, as well as promoting the progress of inflammation.
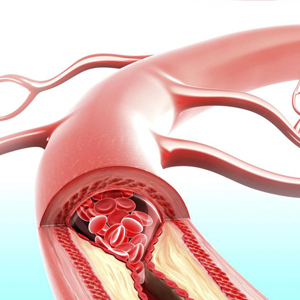
Cardiovascular disease includes the health conditions related to the heart and blood vessels, and it is the cause of one-third of deaths globally. Atherosclerosis is a continuous inflammation of the inner arterial walls with an increase in their permeability causing deposition of plasma lipids and calcium which eventually forms plaques. Atherosclerosis is the most common path to Cardiovascular Disease.
In several studies blood homocysteine level of patients with coronary artery disease was significantly higher than patients without coronary artery disease; in addition, findings show higher homocysteine levels are significantly related to the severity of coronary artery disease, arterial stiffness, and high blood pressure.
How Does Homocysteine Cause Cardiovascular Disease?
Homocysteine impacts vascular endothelium and their smooth muscle cells altering arterial structure and function. It increases the cellular division of vascular smooth muscles, causes endothelial dysfunction, increases oxidative damage, alters collagen synthesis, and deteriorates arterial wall elasticity.
Studies demonstrated that homocysteine is able to initiate an inflammatory response in vascular smooth muscle cells by stimulating CRP (an inflammatory marker) production.
High homocysteine level contributes to lower endothelial production and bioavailability of nitric oxide which is a strong relaxing factor for vessels. There is also strong evidence that increased homocysteine level promotes oxidation. Other studies found that Homocysteine promotes the coagulation process.
Another common cause of cardiovascular diseases is high blood pressure or hypertension. While multiple factors may contribute to the development of hypertension, the association of homocysteine with blood pressure deserves to be noted.
Experimental and animal studies show that high blood pressure could result from high blood homocysteine. Homocysteine may elevate blood pressure in different ways such as its adverse effect on the integrity of vascular endothelium, oxidative stress, and reduced available nitric oxide (vasodilator). Observational human studies found vasodilation impairment in both temporary and chronic cases of hyperhomocysteinemia (High blood Homocysteine level). Homocysteine has been positively linked to both high diastolic and systolic blood pressure.
Homocysteine Levels & Its Impact On The Brain & Nervous System
In recent years, epidemiological studies have found an association between homocysteine level and neurodegenerative disorders. These studies suggest that homocysteine can initiate nerve damage through the oxidative process, DNA Damage, and promoting self-death in neurons cells. Also, an increase in the amount of Homocysteine after head injuries and stroke is related to the release of catecholamines. High catecholamine levels in the blood are associated with stress and depression. Catecholamines also play an important role in regulating heart rate, blood pressure, and blood glucose.
The brain can only metabolize the Homocysteine by converting it back to Methionine using an enzyme called methionine synthase. For this Enzyme to work adequate amount of methylcobalamin ( B12 ) and folate is necessary. It should be noted that the level of 5 tetrahydrofolates (5 MTHF- biologically active form of folate) in the cerebrospinal fluid is 3 times that of the plasma level.
In a clinical study patients with major depressive disorder were prescribed 8 weeks of treatment with a biologically active form of b vitamins which included 5 MTHF. The Montgomery-Asberg Depression Rating Scale (MADRS) was used to evaluate the effect of the treatment. Of the active treatment group, 82.4% showed a reduction in homocysteine and demonstrated, on average, a 12-point reduction on the MADRS by week 8, and 42% achieved full remission. These results support the theory of the relation between homocysteine levels and depression and the safety and therapeutic benefit of an active form of B vitamins, particularly in those cases with deficiencies or some degree of metabolic and genetic disorders.
Folic Acid, B6, B12 Vitamins, and Arterial Plaque Formation

The process of forming plaques in the inner lining of arteries is referred to as Atherogenesis. Vascular cells, particularly vascular endothelial cells are especially vulnerable to high levels of Homocysteine, because they are not equipped by the diversity of enzymes found in the liver to metabolize or reverse production of the homocysteine in different ways.
The endothelia cells are only rely on the re-methylation pathway of converting homocysteine to methionine. This pathway is Folate and vitamin B12 dependent. Folic acid and vitamins B12 and B6 are important regulators of Homocysteine metabolism. B-vitamins, especially Folate is able to reduce plaque formation by lowering homocysteine level, inhibiting production of superoxide (free radicals), and increasing the half life of Nitric Oxide (main vasodilator).
Maintaining moderate-to-high serum folate levels has been shown to be associated with a great reduction in acute coronary events, and an increased intake of Folate has been associated with a decreased risk of ischemic stroke. A study of 26,556 smoker men between 50 to 69 years of age showed that a higher intake of Folate contributed to a statistically significantly lower risk of stroke.
Several trials and studies support the beneficial effects of B-vitamin supplementation in the prevention of Cardiovascular Disease. A Swedish study found that the daily use of multivitamin supplementation (containing 400 mcg of Folate) reduced the risk of MI (Myocardial infarction) in women without a previous history of Cardiovascular Disease. According to the conclusion of the study, multivitamin supplementation may help in the primary prevention of MI.
Meta Data analysis of multiple trials suggests that a number of the trials using B vitamin therapy were effective in reducing the risk of stroke, and long-term vitamin B supplementation may be effective in the primary prevention of Cardiovascular Disease. Primary prevention indicates for those without a previous history of Cardiovascular Disease.
The use of B-vitamins for secondary prevention could be an option to prevent the progress of the disease and when statin therapy caused serious adverse effects and should be omitted. Vitamin B therapy may inhibit the progression of atherogenesis by lowering Homocysteine and by other mechanisms such as its antioxidant properties.
The evidence from studies published over the last two decades suggests that the B vitamin therapy offers an inexpensive, non-toxic, and easy method of primary Cardiovascular Disease prevention and secondary prevention by limiting the progression of the disease due to risk factors such as Homocysteine.
Related articles:
- How to Maintain and Restore Healthy Blood Lipids Level
- Vital Scientific Facts to Maintain an Ideal Cardiovascular Health!
- Nutrients And Their Life Changing Effects On Brain Health
Articles and products featured by Health Palace are collected from a variety of sources and are provided as a service by Health Palace. These newsletters, while of potential interest to readers, do not necessarily represent the opinions nor constitute the advice of Health Palace. Presented materials are only for information purposes and do not intent to treat, cure, or prevent any disease.
Select References:
1.Faeh D, Chiolero A, Paccaud F: Homocysteine as a risk factor for cardiovascular disease: should we (still) worry about it?Swiss Med Wkly 2006, 136:745–56.
2.Baszczuk A, Kopczynski Z: Hyperhomocysteinemia in patients with cardiovascular disease [Abstract].Postepy Hig Med Dosw 2014, 68:579.
3.Curro M, Gugliandolo A, Gangemi C, Risitano R, Ientile R, Caccamo D: Toxic effects of mildly elevated homocysteine concentrations in neuronal-like cells.Neurochem Res 2014, 39:1485–95.
4.Shenov V, Mehendale V, Prabhu K, Shetty R, Rao P: Correlation of serum homocysteine levels with the severity of coronary artery disease.Ind J Clin Biochem 2014,29(3):339–44. 10.1007/s12291-013-0373-50.1007/s11064-014-1338-7
5.Carmel R, Jacobsen DW: Homocysteine in health and disease. Edited by: Carmel R, Jacobsen DW. Cambridge: Cambridge UP; 2001:183–93.
6.Wuerthele SE, Yasuda RP, Freed WJ, Hoffer BJ: The effect of local application of homocysteine on neuronal activity in the central nervous system of the rat.Life Sci 1982, 31:2683–91. 10.1016/0024-3205(82)90712-3.
7.Mangge H, Becker K, Fuchs D, Gostner JM: Antioxidants, inflammation and cardiovascular disease.World J Cardiol 2014,6(6):462–77. 10.4330/wjc.v6.i6.462.
8.Veeranna V, Zalawadiya SK, Niraj A, Pradhan J, Ference B, Burack RC, et al.: Homocysteine and reclassification of cardiovascular disease risk.J Am Coll Cardiol 2011, 58:1025–33. 10.1016/j.jacc.2011.05.028.
9.Pang X, Liu J, Zhao J, Mao J, Zhang X, Feng L, et al.: Homocysteine induces the expression of C - reactive protein via NMDAr-ROS-MAPK-NF-κB signal pathway in rat vascular smooth muscle cells.Atherosclerosis 2014, 236:73–81. 10.1016/j.atherosclerosis.2014.06.021.
10.Okura T, Miyoshi K, Irita J, Enomoto D, Nagao T, Kukida M, et al.: Hyperhomocysteinemia is one of the risk factors associated with cerebrovascular stiffness in hypertensive patients, especially elderly males.Nature.com Sci Rep 2014, 4:5663.
11.Xie R, Jia D, Gao C, Zhou J, Sui H, Wei X, et al.: Homocysteine induces procoagulant activity of red blood cells via phosphatidylserine exposure and microparticles generation.Amino Acids 2014, 46:1997–2004. 10.1007/s00726-014-1755-6.
12.Lim U, Cassano PA: Homocysteine and blood pressure in the third national health and nutrition examination survey, 1988–1994.Oxford Journals: Am J Epidemiol 2002, 156:1105–13. 10.1093/aje/kwf157.
13.Baszczuk A, Kopczyński Z, Thielemann A: Endothelial dysfunction in patients with primary hypertension and hyperhomocysteinemia [abstract].Postepy Hig Med Dosw 2014, 68:91–100.
14.Vijetha Shenoy,Veena Mehendale, Krishnananda Prabhu, Ranjan Shetty, Pragna Rao: Correlation of Serum Homocysteine Levels with the Severity of Coronary Artery Disease. Indian Journal of Clinical Biochemistry July 2014, Volume 29, Issue 3, pp 339–344.
15.Milan Obradovic, Bozidarka L Zaric, Mohamed A Haidara, Esma R. Isenovic : Link between Homocysteine and Cardiovascular Diseases. Cardiovascular Pharmacology (J Li, Section Editor) 18 December 2017.
16.Jakubowski H. Homocysteine thiolactone: metabolic origin and protein homocysteinylation in humans. J Nutr 2000;130:377S–381S.
17.Steed MM, Tyagi SC. Mechanisms of cardiovascular remodeling in hyperhomocysteinemia. Antioxid Redox Signal 2011;15:1927–1943.
18.Becker JS, Adler A, Schneeberger A, et al. Hyperhomocysteinemia, a cardiac metabolic disease: role of nitric oxide and the p22phox subunit of NADPH oxidase. Circulation 2005;111:2112–2118.
19.Tyagi N, Sedoris KC, Steed M, Ovechkin AV, Moshal KS, Tyagi SC. Mechanisms of homocysteine-induced oxidative stress. Am J Physiol Heart Circ Physiol 2005;289:H2649–H2656.
20.Hayden MR, Tyagi SC. Homocysteine and reactive oxygen species in metabolic syndrome, type 2 diabetes mellitus, and atheroscleropathy: the pleiotropic effects of folate supplementation. Nutr J 2004;3:4.
21.Welch GN, Upchurch GRJ, Loscalzo J. Homocysteine, oxidative stress, and vascular disease. Hosp Pract (Minneap) 1997;32:81–92.
22.Distrutti E, Mencarelli A, Santucci L, et al. The methionine connection: homocysteine and hydrogen sulfide exert opposite effects on hepatic microcirculation in rats. Hepatology 2008;47:659–667.
23.Su SJ, Huang LW, Pai LS, Liu HW, Chang KL. Homocysteine at pathophysiologic concentrations activates human monocyte and induces cytokine expression and inhibits macrophage migration inhibitory factor expression. Nutrition 2005;21:994–1002.
24.Holven KB, Aukrust P, Retterstol K, Hagve TA, Mørkrid L, Ose L, Nenseter MS. Increased levels of C-reactive protein and interleukin-6 in hyperhomocysteinemic subjects. Scand J Clin Lab Invest 2006;66:45–54.
25.Gori AM, Corsi AM, Fedi S, et al. A proinflammatory state is associated with hyperhomocysteinemia in the elderly. Am J Clin Nutr 2005;82:335–341.
26.Skurk C, Walsh K. Death receptor induced apoptosis: a new mechanism of homocysteine-mediated endothelial cell cytotoxicity. Hypertension 2004;43:1168–1170.
27.Suhara T, Fukuo K, Yasuda O, et al. Homocysteine enhances endothelial apoptosis via upregulation of Fas-mediated pathways. Hypertension 2004;43:1208–1213.
28.Upchurch GRJ, Welch GN, Fabian AJ, Freedman JE, Johnson JL, Keaney JFJ, Loscalzo J. Homocyst(e)ine decreases bioavailable nitric oxide by a mechanism involving glutathione peroxidase. J Biol Chem 1997;272:17012–17017.
29.Romerio SC, Linder L, Nyfeler J, Wenk M, Litynsky P, Asmis R, Haefeli WE. Acute hyperhomocysteinemia decreases NO bioavailability in healthy adults. Atherosclerosis 2004;176:337–344.
30.Sauls DL, Wolberg AS, Hoffman M. Elevated plasma homocysteine leads to alterations in fibrin clot structure and stability: implications for the mechanism of thrombosis in hyperhomocysteinemia. J Thromb Haemost 2003;1:300–306.
31.Undas A, Brozek J, Jankowski M, Siudak Z, Szczeklik A, Jakubowski H. Plasma homocysteine affects fibrin clot permeability and resistance to lysis in human subjects. Arterioscler Thromb Vasc Biol 2006;26:1397–1404.
32.Ravnskov U, McCully KS. Review and Hypothesis: vulnerable plaque formation from obstruction of Vasa vasorum by homocysteinylated and oxidized lipoprotein aggregates complexed with microbial remnants and LDL autoantibodies. Ann Clin Lab Sci 2009;39:3–16.
33.Alfthan G, Aro A, Gey KF. Plasma homocysteine and cardiovascular disease mortality. Lancet 1997;349:397.
34.Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ 2002;325:1202–1206.
35.Wald DS, Wald NJ, Morris JK, Law M. Folic acid, homocysteine, and cardiovascular disease: judging causality in the face of inconclusive trial evidence. BMJ 2006;333:1114–1117.
36.Humphrey LL, Fu R, Rogers K, Freeman M, Helfand M. Homocysteine level and coronary heart disease incidence: a systematic review and meta-analysis. Mayo Clin Proc 2008;83:1203–1212.
37.Zylberstein DE, Bengtsson C, Björkelund C, Landaas S, Sundh V, Thelle D, Lissner L. Serum homocysteine in relation to mortality and morbidity from coronary heart disease: a 24-year follow-up of the population study of women in Gothenburg. Circulation 2004;109:601–606.
38.Tawakol A, Omland T, Gerhard M, Wu JT, Creager MA. Hyperhomocyst(e)inemia is associated with impaired endothelium-dependent vasodilation in humans. Circulation 1997;95:1119–1121.
39.Mech AW, Farah A AffiliationsThe Journal of Clinical Psychiatry [29 Mar 2016, 77(5):668-671] .Randomized Controlled Trial, Journal Article. 10.4088/JCP.15m10166.
40.McCully KS. Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. Am J Pathol 1969;56:111–128.
41.Suzuki K, Murakami K, Tomita T, et al. A case of young adult presenting with cerebral infarction caused by homocystinuria. No To Shinkei 2004;56:781–784.
42.Rasouli ML, Nasir K, Blumenthal RS, Park R, Aziz DC, Budoff MJ. Plasma homocysteine predicts progression of atherosclerosis. Atherosclerosis 2005;181:159–165.
43.Kullo IJ, Li G, Bielak LF, et al. Association of plasma homocysteine with coronary artery calcification in different categories of coronary heart disease risk. Mayo Clin Proc 2006;81:177–182.
44.Held C, Sumner G, Sheridan P, et al. Correlations between plasma homocysteine and folate concentrations and carotid atherosclerosis in high-risk individuals: baseline data from the Homocysteine and Atherosclerosis Reduction Trial (HART). Vasc Med 2008;13:245–253.
45.Shukla N, Angelini GD, Jeremy JY. The administration of folic acid reduces intravascular oxidative stress in diabetic rabbits. Metabolism 2008;57:774–781.
46.Kolling J, Scherer EB, da Cunha AA, da Cunha MJ, Wyse ATS. Homocysteine induces oxidative-nitrative stress in heart of rats: prevention by folic acid. Cardiovasc Toxicol 2011;11:67–73.
47.Doshi S, McDowell I, Moat S, Lewis M, Goodfellow J. Folate improves endothelial function in patients with coronary heart disease. Clin Chem Lab Med 2003;41:1505–1512.
48.Shirodaria C, Antoniades C, Lee J, et al. Global improvement of vascular function and redox state with low-dose folic acid: implications for folate therapy in patients with coronary artery disease. Circulation 2007;115:2262–2270.
49.Yilmaz H, Sahin S, Sayar N, et al. Effects of folic acid and N-acetylcysteine on plasma homocysteine levels and endothelial function in patients with coronary artery disease. Acta Cardiol 2007;62:579–585.
50.Title LM, Ur E, Giddens K, McQueen MJ, Nassar BA. Folic acid improves endothelial dysfunction in type 2 diabetes–an effect independent of homocysteine-lowering. Vasc Med 2006;11:101–109.
51.Das UN. Folic acid says NO to vascular diseases. Nutrition 2003;19:686–692.
52.Moens AL, Champion HC, Claeys MJ, et al. High-dose folic acid pretreatment blunts cardiac dysfunction during ischemia coupled to maintenance of high-energy phosphates and reduces postreperfusion injury. Circulation 2008;117:1810–1819.
53.Moens AL, Vrints CJ, Claeys MJ, Timmermans JP, Champion HC, Kass DA. Mechanisms and potential therapeutic targets for folic acid in cardiovascular disease. Am J Physiol Heart Circ Physiol 2008;294:H1971–H1977.
54.He L, Zeng H, Li F, et al. Homocysteine impairs coronary artery endothelial function by inhibiting tetrahydrobiopterin in patients with hyperhomocysteinemia. Am J Physiol Endocrinol Metab 2010;299:E1061–E1065.
55.Marcucci R, Zanazzi M, Bertoni E, et al. Vitamin supplementation reduces the progression of atherosclerosis in hyperhomocysteinemic renal-transplant recipients. Transplantation 2003;75:1551–1555.
56.Hodis HN, Mack WJ, Dustin L, et al. High-dose B vitamin supplementation and progression of subclinical atherosclerosis: a randomized controlled trial. Stroke 2009;40:730–736.
57.Holmquist C, Larsson S, Wolk A, de Faire U. Multivitamin supplements are inversely associated with risk of myocardial infarction in men and women–Stockholm Heart Epidemiology Program (SHEEP). J Nutr 2003;133:2650–2654.
58.Rautiainen S, Akesson A, Levitan EB, Morgenstern R, Mittleman MA, Wolk A. Multivitamin use and the risk of myocardial infarction: a population-based cohort of Swedish women. Am J Clin Nutr 2010;92:1251–1256.
59.Antoniades C, Antonopoulos AS, Tousoulis D, Marinou K, Stefanadis C. Homocysteine and coronary atherosclerosis: from folate fortification to the recent clinical trials. Eur Heart J 2009;30:6–15.
60.Albert CM, Cook NR, Gaziano JM, et al. Effect of folic acid and B vitamins on risk of cardiovascular events and total mortality among women at high risk for cardiovascular disease: a randomized trial. JAMA 2008;299:2027–2036.
61.The Heart Outcomes Prevention Evaluation (HOPE) 2 Investigators. Homocysteine lowering with folic acid and B vitamins in vascular disease. N Engl J Med 2006;354:1567–1577.
62.Wang X, Qin X, Demirtas H, et al. Efficacy of folic acid supplementation in stroke prevention: a meta-analysis. Lancet 2007;369:1876–1882.
63.Mark SD, Wang W, Fraumeni JFJ, et al. Lowered risks of hypertension and cerebrovascular disease after vitamin/mineral supplementation: the Linxian Nutrition Intervention Trial. Am J Epidemiol 1996;143:658–664.
64.Liem A, Reynierse-Buitenwerf GH, Zwinderman AH, Jukema JW, van Veldhuisen DJ. Secondary prevention with folic acid: results of the Goes extension study. Heart 2005;91:1213–1214.
65.Lee M, Hong KS, Chang SC, Saver JL. Efficacy of homocysteine-lowering therapy with folic acid in stroke prevention: a meta-analysis. Stroke 2010;41:1205–1212.
66.Vianna ACA, Mocelin AJ, Matsuo T, et al. Uremic hyperhomocysteinemia: a randomized trial of folate treatment for the prevention of cardiovascular events. Hemodial Int 2007;11:210–216.
67.Ji Y, Tan S, Xu Y, et al. Vitamin B supplementation, homocysteine levels, and the risk of cerebrovascular disease: a meta-analysis. Neurology 2013;81:1298–1307.
68.Galan P, Kesse-Guyot E, Czernichow S, Briancon S, Blacher J, Hercberg S, SU.FOL.OM3 Collaborative Group. Effects of B vitamins and omega 3 fatty acids on cardiovascular diseases: a randomised placebo controlled trial. BMJ 2010;341:c6273.
69.Bazzano LA, Reynolds K, Holder KN, He J. Effect of folic acid supplementation on risk of cardiovascular diseases: a meta-analysis of randomized controlled trials. JAMA 2006;296:2720–2726.
70.Nakazato R, Gransar H, Berman DS, et al. Statins use and coronary artery plaque composition: results from the International Multicenter CONFIRM Registry. Atherosclerosis 2012;225:148–153.
71.Balazs Debreceni Department of Biochemistry and Medical Chemistry, Medical School, University of Pecs, Pecs, Hungary. Laszlo Debreceni, Heart Disease Research Foundation, Brooklyn, NY, USA; First published: 23 April 2014; 10.1111/1755-5922.12064
72.Paul Ganguly and Sreyoshi Fatima Alam, Nutrition Journal201514:6; 10 January 2015 .doi.org/10.1186/1475-2891-14-6
Designs for Health Homocysteine Supreme 60 Veg Capsules | Integrative Therapeutics Active B Complex 60 Veg Capsules | BioMed Optimum B12 MeF 60 Lozenges |
 |  |  |
| • Helps in tissue formation • Helps with liver, skin and immune function • Helps in the formation of red blood cells • Helps the body to metabolize carbohydrates, fats and proteins ...Read more | Pure, hypoallergenic, vegetarian B-complex formula. • Features the active forms of vitamins B2, B6, B12, and folate • Contains Quatrefolic brand L-Methylfolate, the bioactive form of folate • Supports healthy methylation* ...Read more | Optimum
B12 MeF is a high potency vitamin B12 (methylcobalamin) and folate
(L-5-Methyltetrahydrofolate, L-5-MTHF) formula. This quick dissolve
sublingual lozenge offers ...Read more |
NFH Cardio SAP 60 Veg Capsules | Aor Maxmethyl 90 Veg Capsules | Designs for Health CatecholaCalm 90 Veg Capsules |
 |  |
|
| Elevated
blood homocysteine is also thought to relate to onset of diseases of
the brain and kidneys and to diabetic complications. | • Decreases dangerous levels of homocysteine • Lowers the risk of cardiovascular disease • Protects against damaged blood vessels • Slows the aging process ...Read More | •Helps to temporarily promote relaxation •Helps to maintain proper muscle function |
 |  |  |
Recent Posts
-
Maintain A Healthy Heart Rhythm With Integrative Medicine
Maintain A Healthy Heart Rhythm With Integrative Medicine;Usually, abnormal heart rate or arrhythmi …4th Feb 2021 -
How To Protect Against COVID-19
Coronaviruses are a large group of viruses that cause many common human and animal infections. In hu …30th Jun 2020 -
How to Prevent Gallstones from Forming? | Natural Supplements for Gallstones
How To Prevent Gallstone Formation?Gallstones are hard deposits made of cholesterol or bilirubin f …4th Mar 2020